MEDICARE GUIDELINES
How to Enroll in Medicare
Enrolling in Medicare Part A and Part B (Original Medicare) is typically the first step in enrolling in Medicare.
You need to sign up for Part A and/or Part B. Call Social Security at 1-800-772-1213 from 7 a.m. to 7 p.m., Monday-Friday (TTY: 1-800-325-0778). Or visit medicare.gov to apply online.
If you worked for a railroad, then you need to call 1-877-772-5772 to learn more about signing up.
You'll be automatically enrolled in Part A and Part B. Medicare will send you a card before you turn 65 with information on how to disenroll from Part B, if you wish.
If you don't receive your Medicare card a few months before your 65th birthday, call 1-800-772-1213, from 7 a.m. to 7 p.m. Monday-Friday (TTY: 1-800-325-0778).
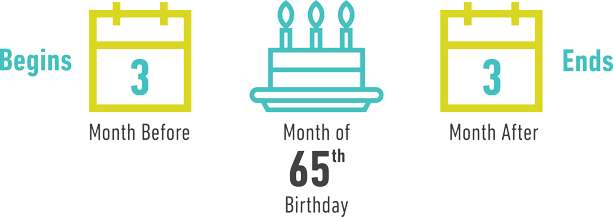
Initial Enrollment Period
You become eligible to sign up for Medicare during a seven-month period called the Initial Enrollment Period (IEP). This covers the three months before you turn 65, the month you turn 65, and three months after you turn 65. During IEP, you’re eligible to enroll in Medicare Part A, Medicare Part B, Medicare Advantage (Part C) or a Part D prescription drug plan. If you want your coverage to start the month of your 65th birthday, you must enroll at least one month before your birthday month. If you don’t enroll in Medicare Part B or Part D when you first become eligible, you may have to pay a premium penalty if you enroll later.
General Enrollment Period
If you don't sign up for Part A and/or Part B during the Initial Enrollment Period when you are first eligible, you can sign up during the General Enrollment Period between January 1 and March 31 each year, for coverage beginning July 1.
Need Help?
1-877-704-7864
(TTY: 711)
Questions? Connect with Us
Get Info Kit
Annual Enrollment Periods
Your health plan coverage needs may change from year to year. And you may decide that another type of plan is more appropriate for your situation. So Medicare provides times each year for you to make changes to your plan.
Annual Election Period:
October 15 – December 7
During this time, you can make changes to your plan that will take effect on January 1 the new plan year. All enrollment, disenrollment or plan change options are available to you during this time. Here are some examples:
- Change from Original Medicare to a Medicare Advantage plan or vice versa
- Switch from a Cost plan with Part D to another Cost plan with Part D or an alternative private plan like Medicare Advantage
- Switch from one Medicare Advantage plan to another Medicare Advantage plan or a Cost plan
- Switch from one Medicare Prescription Drug plan to another Medicare Prescription Drug plan or a Medicare Advantage plan or Cost plan with Part D
Medicare Advantage Open Enrollment Period:
January 1 – March 31
If you're enrolled in a Medicare Advantage plan, you have a one-time opportunity to:
- Switch to a different Medicare Advantage plan
- Drop your Medicare Advantage plan and return to Original Medicare (Part A and Part B)
- Sign up for a stand-alone Medicare Part D Prescription Drug Plan (if you return to Original Medicare)
Special Enrollment Periods (SEP)
A Special Enrollment Period (SEP) allows you to avoid the Medicare Part B penalty for late enrollment. You may qualify if:
- You delayed enrollment in Medicare Part B because you or your spouse has medical coverage through an employer or union with more than 20 employees, or
- You canceled Part B coverage because you went back to work and have group medical coverage.
You have eight months to take action. Your SEP begins when your employer coverage ends or when your employment ends, whichever is first. Contact Social Security or your employer for more information. If you are age 65 and have COBRA through a previous employer, you should enroll in Medicare Part B. You will not get an SEP when COBRA ends.Be sure to enroll in Part B during the first eight months of your COBRA coverage to avoid the late enrollment penalty.
If you're already enrolled in Medicare and want to enroll in a Medicare Advantage (Part C) or Part D drug plan, you can enroll during the Annual Election Period (October 15 to December 7). Outside of this period, you can enroll if you meet a Special Enrollment Period requirement such as:
- You move outside your plan's service area
- You're eligible for Medicaid
- You qualify for Extra Help with Medicare prescription drug costs
- You want to switch to a plan with a 5-star overall quality rating
- Your current plan's government contract ends or the plan goes out of business
- You lose prescription drug coverage from an employer or union or your drug coverage is no longer as good as the standard Part D benefit
Other Enrollment Periods
Typically, you can join a Medicare Cost plan anytime the plan is accepting new members. If you're newly eligible for Medicare, you can enroll anytime during your seven-month Initial Enrollment Period as long as you are enrolled in Medicare Part B. However, if you're currently enrolled in a Medicare Advantage plan or a Part D drug plan, you must first disenroll from that plan before enrolling in a Cost plan.
The best time to enroll in a Medigap plan is during the six-month Medigap open enrollment period which begins the month you're 65 and you are enrolled in Part B. If you apply for coverage outside of your open enrollment period, you may be required to provide your health history and be medically underwritten. This means you could be denied coverage, or it may cost more.
